Dr Jim Allison
2018 Nobel Prize Winner
Last Viewed March 28 2021
Simplified Note
Video Time Stamp 7mins
CTLA-4 & CD28 are protein-ligand receptors that sit on the surface of a T-Cell. They each compete to bind with the costimulatory B7 ligand on the surface of an APC cell (Antigen Presenting Cell) APC cells are the innate immune systems messenger cells and the B7 is the stimulating ligand ie ie it activates.
- CD28 binding with a B7 activates the T-Cells
- CTLA-4 binding with a B7 deactivates the T-Cell
- B7 (B7 1 & B7 2) are costimulatory ligand molecules -sole purpose is to turn on the T-cells
Note – Ipi/Nivo Treatment: (Immunotherapy)
- Ipilimumab is an anti-CTLA-4 (interventional-Blocking) drug
- Nivolumab is an anti-PD-1 (interventional-Blocking) drug
Shomu Tuts
CSIR Exam preps
Immunohistochemistry lecture – This lecture explains about the immunohistochemistry principle and procedure and why we use it to identify a specific type of antigen from tissue samples. For more information, log on to- http://www.shomusbiology.com/ Get Shomu’s Biology DVD set here- http://www.shomusbiology.com/dvd-store/ Download the study materials here- http://shomusbiology.com/bio-material… Remember Shomu’s Biology is created to spread the knowledge of life science and biology by sharing all this free biology lectures video and animation presented by Suman Bhattacharjee in YouTube. All these tutorials are brought to you for free. Please subscribe to our channel so that we can grow together. You can check for any of the following services from Shomu’s Biology- Buy Shomu’s Biology lecture DVD set- www.shomusbiology.com/dvd-store Shomu’s Biology assignment services – www.shomusbiology.com/assignment -help Join Online coaching for CSIR NET exam – www.shomusbiology.com/net-coaching
Shomu’s Biology
841K subscribers
This DNA mutation lecture explains about types of point mutations like nonsense mutation, missense mutation, silent mutation etc.
A mutation is a everlasting exchange somewhere in a DNA sequence. DNA is the unit of heredity of all organisms, so this means that mutations can most often be handed on to offspring. Mutations do not have got to be bad. Some are worthy, whilst others are impartial or don’t have any effect. There are a lot of one of a kind categories of mutations, however in this lesson we can center of attention on factor mutations, or these attributable to a metamorphosis in a single or a fewnucleotides at a single area in a DNA sequence.
A mutation that includes a single nucleotide and may consist of lack of a nucleotide, substitution of a nucleotide for another, or the insertion of an extra nucleotide.
For instance, sickle-mobile disorder is triggered with the aid of a single factor mutation (a missense mutation) within the beta-hemoglobin gene at role 6 that converts a GAG codon into GTG, which encodes the amino acid valine as a substitute than glutamic acid.
For more information, log on to-
http://www.shomusbiology.com/
Get Shomu’s Biology DVD set here-
http://www.shomusbiology.com/dvd-store/
Download the study materials here-
http://shomusbiology.com/bio-material…
Remember Shomu’s Biology is created to spread the knowledge of life science and biology by sharing all this free biology lectures video and animation presented by Suman Bhattacharjee in YouTube. All these tutorials are brought to you for free. Please subscribe to our channel so that we can grow together. You can check for any of the following services from Shomu’s Biology-
Buy Shomu’s Biology lecture DVD set- www.shomusbiology.com/dvd-store
Shomu’s Biology assignment services – www.shomusbiology.com/assignment -help
Join Online coaching for CSIR NET exam – www.shomusbiology.com/net-coaching
We are social. Find us on different sites here-
Our Website – www.shomusbiology.com
Facebook page- https://www.facebook.com/ShomusBiology/
Twitter – https://twitter.com/shomusbiology
SlideShare- www.slideshare.net/shomusbiology
Google plus- https://plus.google.com/1136485849827…
LinkedIn – https://www.linkedin.com/in/suman-bha…
Youtube- https://www.youtube.com/user/TheFunsuman
Thank you for watching
This video discusses about properties of antigens and antibodies and their interaction pattern and also the importance of antigen antibody complex in detecting diseases by immunoassay.
An immune complex is formed from the integral binding of an antibody to a soluble antigen. The bound antigen and antibody act as a specific epitope, and is referred to as a singular immune complex. After an antigen-antibody reaction, the immune complexes can be subject to any of a number of responses, including complement deposition, opsonization, phagocytosis, or processing by proteases. Red blood cells carrying CR1-receptors on their surface may bind C3b-decorated immune complexes and transport them to phagocytes, mostly in liver and spleen, and return to the general circulation.
Immune complexes may themselves cause disease when they are deposited in organs, e.g. in certain forms of vasculitis. This is the third form of hypersensitivity in the Gell-Coombs classification, called Type III hypersensitivity.
Immune complex deposition is a prominent feature of several autoimmune diseases, including systemic lupus erythematosus, cryoglobulinemia, rheumatoid arthritis, scleroderma and Sjögren’s syndrome.
Shomu’s Biology
841K subscribers
Antigen presenting cells or APCs – This lecture explains about the properties of Professional antigen presenting cells such as macrophage, dendritic cells and B cells. It also explains the importance of antigen presenting cells or APC to engulf a pathogen through phagocytosis and then presenting it to the whole immune system so that cell mediated and humoral immune response can build up.
Mature, naive B- and T cells, as well as precursors of APC (antigen presenting cells, including monocytes/macrophages and dendritic cells) from the bone marrow emigrate from the central lymphatic organs. Lymphocytes travel mainly via the bloodstream. APC leave the bloodstream to widely roam tissues. Eventually, all types of cells meet again at the peripheral lymphatic organs: lymph nodes, GALT/Peyer plaques and tonsils, BALT and spleen.
Lymph nodes seem static in the microscope, but should better be compared to the transit area of a big international airport, with oodles of cells arriving and leaving all the time. Lymph nodes have several inlets and an outlet. Afferent lymphatic vessels reaching the most peripheral lymph nodes transport the interstitial fluid filtrated from blood capillaries. With the lymph flow, dendritic cells loaded with ingested material drift to the lymph nodes, e. g., Langerhans cells from the skin. In case of an infection, lymph flow increases dramatically, carrying with it pathogens and their antigenic molecules, outside and inside of activated macrophages and dendritic cells. Thus, a lymph node is a local command center with continuous real-time information on the antigenic situation in the periphery. From the blood, lymphocytes constantly enter the lymph node via specialized high endothelial venules. B cells migrate to areas near the cortex, and, if activated, form follicles with germinal centers. There, specialized “follicular dendritic cells” immobilize immune complexes with their Fc- and complement receptors, so that the antigens are “visible” to the proliferating B cells. T cells wander to adjacent paracortical areas. Some activated B cells that already have differentiated to plasma cells, and more macrophages, sit in the lymph node’s medulla. Each lymph node has an efferent vessel connecting to the next lymph node and, eventually, via the thoracic duct to the blood.
(Caution: “dendritic cells” and “follicular dendritic cells” are completely different cell types that obtained similar names (dendritic = tree-like) because of their morphological appearance. Dendritic cells are specialized APC ingesting antigen in the periphery and presenting processed antigen on MHC II to T cells. Follicular dendritic cells sit in germinal centers and use complement receptors and Fc receptors to fix antigen-containing immune complexes on their outer surface for B cells to see.)
For more information, log on to-
http://www.shomusbiology.com/
Get Shomu’s Biology DVD set here-
http://www.shomusbiology.com/dvd-store/
Download the study materials here-
http://shomusbiology.com/bio-material…
Remember Shomu’s Biology is created to spread the knowledge of life science and biology by sharing all this free biology lectures video and animation presented by Suman Bhattacharjee in YouTube. All these tutorials are brought to you for free. Please subscribe to our channel so that we can grow together. You can check for any of the following services from Shomu’s Biology-
Buy Shomu’s Biology lecture DVD set- www.shomusbiology.com/dvd-store
Shomu’s Biology assignment services – www.shomusbiology.com/assignment -help
Join Online coaching for CSIR NET exam – www.shomusbiology.com/net-coaching
We are social. Find us on different sites here-
Our Website – www.shomusbiology.com
Facebook page- https://www.facebook.com/ShomusBiology/
Twitter – https://twitter.com/shomusbiology
SlideShare- www.slideshare.net/shomusbiology
Google plus- https://plus.google.com/1136485849827…
LinkedIn – https://www.linkedin.com/in/suman-bha…
Youtube- https://www.youtube.com/user/TheFunsuman
Thank you for watching the lecture on Antigen presenting cells.
B Cells are one of 3 types of Antigen Presenting Cells (APC) –
B Cell, Dendritic, Cells & Macrophages
Notes
- Cross talk between T Cells and B Cells
Notes
- Interferon = “IFN”
- Cytokines generate Cross talk between the immuns T Cells and B Cells
- Interferon means to interfere in the replication of viruses or foreign entities
- Cytokines are immune signaling cells – there are many different types
- Interferons are one type of Cytokines
Antigen Presenting Cells consume foreign invaders.
APC consumes foriegn antigens and their pathogens, they digest and showcase a sample of theses antigens at their surface through a receptor called MHC 2.
MHC 2 transports this digested sample from within the APC cell, to the exterior surface, like a warning flag with a sample fragment (Antigen) attached that attracts help. Help can then engage with the antigen and recruit more help from the immune systems Helper T Cells and B Cells.
APC Cells are of 3 types
- Dendritic Cells (DC)
- B Cells
- Macrophages
This Video highlights Macrophages as the APC example.
- All Neucleated Cells have MHC 1 on their surface,
- All APC Cells have MHC 2 as well. The 3 types of APC cells are Macrophages, B Cells, T Cells.
- MHC (1) are receptors on the surface of all neckeated cells.
- MHC receptors provide a presentation of material within the cell to the outside of the cell -a flag or a passport ID
- MHC = Major Histocompatibilty Complex
- MHC 1 is critical, as it is the mechanism that identifies the foreign invader within the cell (like a virus), it converts a sample of this virus material to be displayed / flagged on the cells surface to alert T Cells to destroy it.
- CD8+ T Cells once interaction occurs with the infected cell, the Cell goes through a confirmation process. It the releases perferins that punch holes into the cell surface and then release granzymes to enter via the holes and downgrade the cells dna/destroy the cells nucleus.
- MHC 1 only interests with CD8+ Cyctotoxic Killer T Cells
- MHC 2 only interacts with CD4+ T Helper Cells
MHC 1 attracts immediate Killer T Celll response
MHC 2 recuits the immune system to amplify ie more macrophages, and B Cells to producing plasma that create antibodies that locate the foreign antigens, and also produce memory B cells for use at a later date. ie remember this threat.
MHC2 – When a APC cell and a Helper T Cell bind correctly via its ligands and receptors, this then activates the Helper T Cell to release cytokines (Chemical messengers) such as interleukind and interferon gamma to recruit and amplify the immune response.
Note: APC cells have CD = Cluster Differenttions on their surface. In this example – CD 80 & 86 =CD 40.
Note: Also refers to CD4+ Helper T Cells having CD 28 receptors and CD 40 ligands on its surface to corresponspd /communicate with the APC cell.
Note All these CD’s need to match and bind to create activation.
Note Interleukins, interferons are part of the cytokine family.
Also view
Antigens – Antibodies
Immune system response to foreign entities –
Mutations are mistakes – ie cancers. Pathogens enter the body to invade healthy cells – ie viruses
-Antigens
As explain by a med student
This video is part of the Cancer Research Institute’s series “Immunotherapy: 5 Ways to Stop Cancer.” For more information on treating cancer with immunotherapy, visit http://www.cancerresearch.org.
Monoclonal antibodies, like the drugs Avastin (bevacizumab), Herceptin (trastuzumab), and Rituxin (rituximab), are effective in treating a wide range of cancer types such as lung cancer, breast cancer, lymphoma, and others. By binding to cancer antigens, monoclonal antibodies mark the cells for destruction by the immune system. Clinical trials of more monoclonal antibodies for additional cancer types are ongoing.
-Antibodies
*years ago
Monoclonal antibodies mimic natural proteins found in the body to specifically and effectively target abnormal cells. Dr Martin Kaiser explains how these are being developed to treat myeloma.
Checkpoint Pathway
Comments
MHC Class I Deficiency in Solid Tumors and Therapeutic Strategies to Overcome It
Published 23 June 2021
The immune system plays a critical role in preventing and controlling cancer growth. Anti-tumor immunity relies largely on CD8 T cell-mediated recognition of tumor antigens. Cancers have developed sophisticated strategies to escape immune-mediated control and this includes the downregulation or loss of antigens or the major histocompatibility class (MHC)-I molecules—the molecular structures presenting these antigens. Cancers can also promote an immunosuppressive microenvironment that disables T-cell killing via the expression of immune inhibitory molecules. Immunotherapy, also known as immune checkpoint blockade (ICB), helps the immune system regain control. Therapeutic antibodies targeting the immune inhibitory receptors Programmed Death-1 (PD-1) and Cytotoxic T Lymphocyte Antigen-4 (CTLA-4) induce durable responses in a proportion of patients with melanoma, lung, kidney, bladder and other cancers [1–9]. However, many patients progress while on treatment, and primary treatment resistance remains a major obstacle. Combined immunotherapy (anti-PD1 plus anti-CTLA-4) results in higher objective response rates [2] but is also associated with significant immune-related toxicities that are often severe and can be life-threatening [10,11].
Continue reading – article_deploy/ijms-22-06741-v2.pdf
This video outlines CTLA-4 and PD-L1
CTLA-4 – A moving target
interactions of the ligands with CTLA-4 serve to inhibit T-cell responses, although the precise mechanisms are not fully understood. CTLA-4 interacts with both ligands with higher affinity and avidity than CD28….

Lasted Viewed: 28 March 2021
This explains the purpose and function of our immune system and then focuses on the ICI – CTLA-4 & PD-1 Checkpoint blockades.
alos 10:00 min talks about other Checkpoint mutations
Science ABC
80K subscribers
The immune system (or immunity) can be divided into two types – innate and adaptive immunity. This video has an immune system animation. The innate immune system consists of defenses against infection that are activated instantly as a pathogen attacks. Adaptive immunity (or acquired immunity) is a subsystem of the immune system that contains highly specialised systemic cells and processes that kill pathogens and prevent their growth in the body. Innate vs adaptive immunity: it’s important to realize that innate and adaptive immunity are different. Their differences are explained in the video in layman terms.
Our immune system is a fascinating entity, that functions in quite a unique and efficient manner. Comprising of various types of cells, it is prepared for any kind of breach in the fortress of our body, and is equipped to fight off a staggering number of intruders.
In this video, we give you a brief overview of the immune system, and the basic types of cells involved, along with the function they carry out.
Each cell if the immune system carries out various roles, depending on the kind of threat the body is facing. However, they have certain basic roles which have been explained here.
References
https://ciiid.washington.edu/content/…
http://www.biology.arizona.edu/immuno…
http://sphweb.bumc.bu.edu/otlt/MPH-Mo…
https://med.uth.edu/pathology/files/2…
SUBSCRIBE to get more such science videos!
https://www.youtube.com/channel/UCcN3…
Follow us on Twitter!
Follow us on Facebook!
https://facebook.com/sciabc
Follow our Website!
https://www.scienceabc.com
James Allison and Tasuku Honjo have jointly received the Nobel Prize in physiology or medicine for their work on immune checkpoints. Allison and Honjo set the stage in the 1990s for the current immuno-oncology boom by discovering the cancer-killing potential of CTLA-4 and PD-1, respectively.
Cyctokines
Cross talk – Cellular and chemical messaging
Interferons are cell signaling molecules within our immune system.
They are produced by a cell in response to a pathogen invasion.
- The impacted Cell expresses interferons to alert other cells to prepare against this invasion.
- The expressed interferons also alert the Immune Systems NK -Natural Killer Cells that an invasion is underway.
- NK Cells in turn also produce interferons to stimulate Macrophages – this is known as the “Macrophage Activation Factor”
DNA + RNA
Deoxyribonucleic acid is a polymer composed of two polynucleotide chains that coil around each other to form a double helix carrying genetic instructions for the development, functioning, growth, and reproduction of all known organisms and many viruses. DNA and ribonucleic acid are nucleic acids
Ribonucleic acid, a nucleic acid present in all living cells. Its principal role is to act as a messenger carrying instructions from DNA for controlling the synthesis of proteins, although in some viruses RNA rather than DNA carries the genetic information.
Ribosomes (in the Cytoplasm) make proteins
Stretches of Nucleotide Repeats within the genome
>>>>>
Khan Academy
Introduction to nucleic acids (e.g. DNA and RNA) and Nucleotides. Click this link to view the video
Nucleotides are the building blocks (Backbones) of both DNA & RNA. They are groups of arranged Nucleic Acids (Oxygen, Carbons, Nitrogens)
DNA Pairing = Apples in the Tree = A&T, and Car in the Garage = C&G
RNA Paring = Apples Under the tree = A&U and Car in the Garage = C&G
Types of RNA –mRNA (Messenger) – rMNA (Ribsomal) – tRNA (Transfer)
Why is RNA just as cool as DNA?
Join the Amoeba Sisters as they compare and contrast RNA with DNA and learn why DNA should be sharing the limelight! Video has updated handout here https://www.amoebasisters.com/handouts and is updated from the old version of this video:
Protein Synthesis (Updated)
Explore the steps of transcription and translation in protein synthesis! This video explains several reasons why proteins are so important before explaining the roles of mRNA, rRNA, and tRNA in the steps of protein synthesis! Expand details for contents and resources.
DNA Replication Updated
Explore the steps of DNA replication, the enzymes involved, and the difference between the leading and lagging strand! This video is an update from our old DNA replication video with nearly the same script but added detail and improved art!
mRNA, tRNA, and rRNA function
Immunotherapy
-How it works
By Batu Biologics’ ValloVax™ Technology
-Trial and Results
Thyroid dysfunction is one of the most common adverse events that may occur during anti–PD‐1 immunotherapy . . . continue reading
The investigators followed the patients for a median of 14.9 months. Of all patients, 20% (34 patients) developed subclinical thyroid dysfunction, and 12% (20 patients) developed overt thyroid dysfunction. Sixteen percent (27 patients) had preexisting thyroid dysfunction, a group that included 9 patients with hyperthyroidism and 18 patients with hypothyroidism. Of these 27 patients, 22 were categorized as having subclinical thyroid dysfunction based on THS values. Of all patients in the study, 48% (80 patients) did not develop thyroid dysfunction. The researchers were unable to establish thyroid dysfunction status in 7 patients “due to missing TSH values,” according to the paper.
Overall survival was higher among patients who developed overt thyroid dysfunction during treatment (hazard ratio [HR], 0.18; CI 95%, 0.04‐0.76, P =.020) compared with patients who did not have overt thyroid dysfunction — and so was progression-free survival (HR, 0.39; 0.15‐0.998; P =.050).
The 1-year overall survival rate among those who developed overt thyroid dysfunction during treatment was 94% compared with 59% among those who did not have overt thyroid dysfunction. One‐year progression-free survival rates were 64% and 34%, respectively.
There was no increase in survival linked to acquired subclinical thyroid dysfunction or preexisting thyroid dysfunction.
Patients with ATAb levels above the median at baseline did not have longer overall survival or progression-free survival. However, overall survival rates were higher for those who had ATAb levels that were above the median during treatment compared with those whose ATAb levels were below the median during treatment, at 83% vs 49%, respectively, at 1 year. Progression-free survival rates at 1 year were also higher for patients with above-the-median ATAb levels during treatment compared with levels below the median during treatment, at 54% vs 20%.
Long-Term Outcomes With PD-1 Inhibitor Treatment and Response to Retreatment in Advanced Melanoma
The estimated 3-year overall survival from time of complete response was 82.7%. Among patients who achieved and remained in complete response for 1 year after it was identified, the conditional probability of remaining in complete response for 2 more years was 83.3%. No significant association was observed between treatment duration and relapse risk.
The investigators concluded, “In our cohort, most patients discontinued treatment at the time of complete response. Most complete responses were durable, but the probability of treatment failure was 27% at 3 years. Responses to retreatment were infrequent. The optimal duration of treatment after complete response is not yet established.” …Red Complete findings…
CAR T-Cell Therapy: How Does It Work?
CAR T-cell therapy, like all forms of cancer immunotherapy, seeks to sharpen and strengthen the immune system’s inherent cancer-fighting powers. It involves treating patients with modified versions of their own immune system T cells – white blood cells that help protect the body from disease …
CAR T-cell therapy is a kind of cellular therapy, which uses a patient’s own immune system cells to rally an attack on cancer. They’re made by removing a specific set of cells from the blood, modifying them in a lab to intensify the immune system’s natural response to cancer, and re-injecting them into the patient. CAR T cells are a form of cellular therapy that has produced exceptional results in some patients and is being tested against a variety of different cancer types.
Both CAR T-cell therapies and therapeutic cancer vaccines are considered immunotherapies because they work with the immune system to fight cancer. However, they differ from other immunotherapy agents known as immune checkpoint inhibitors, which aim to lower the barriers that can keep the anti-cancer immune response in check. . . Learn more
-Treatments
Society for Immunotherapy of Cancer
4.44K subscribers
Created by Dr. Samir N. Khleif (Georgetown Lombardi Comprehensive Cancer Center), in partnership with the Society for Immunotherapy of Cancer (SITC) and Cancer Support Community, IMMUNOTHERAPY: The Path to a Cancer Cure explains the interplay between the immune system and cancer; mechanisms underlying immune-based agents; and different approaches to cancer immunotherapeutics.
Patients: Watch the Patient version of this video here:
Various
Balversa (Erdafitinib), First-in-Class FGFR Kinase Inhibitor,
Approved for Patients with Metastatic Urothelial Carcinoma and FGFR Mutations
2019 Payers’ Guide Mid-Year Addendum – Select Drug Profiles read article
Biomarker – Mutations by type
Comments
Source link
About IDH and Malignancies
IDHs are critical metabolic enzymes that help to break down nutrients and generate energy for cells. When mutated, IDH creates a molecule that alters the cell’s genetic programming and prevents cells from maturing, 2-hydroxyglutarate (“2-HG”). Reduction in 2-HG levels can be used as a marker of target engagement by an IDH inhibitor. IDH1 or IDH2 mutations are common genetic alterations in various types of blood and solid tumors, including acute myeloid leukemia (“AML”) with approximately 20% of patients having mutant IDH genes, myelodysplastic syndrome (MDS), myeloproliferative neoplasms (MPNs), low-grade glioma and intrahepatic cholangiocarcinoma (“IHCC”). Mutant IDH isoform switching, either from cytoplasmic mutant IDH1 to mitochondrial mutant IDH2, or vice versa, is a mechanism of acquired resistance to IDH inhibition in AML and cholangiocarcinoma.1,2,3 Currently, the U.S. Food and Drug Administration (FDA) has approved one drug for IDH1 mutation and one drug for IDH2 mutation, but no dual inhibitor targeting both IDH1 and IDH2 mutants has been approved.
A Study of Erdafitinib in Participants With Advanced Solid Tumors and Fibroblast Growth Factor Receptor (FGFR) Gene Alterations
ClinicalTrials.gov: Brief Summary: Drug: Erdafitinib:
The purpose of this study is to evaluate the efficacy of erdafitinib in terms of overall response rate (ORR) in participants with advanced solid tumors with fibroblast growth factor receptor (FGFR) mutations and gene fusions. read trial study
What is FGFR
What is considered a high tumor mutation burden?
Evaluation of tumor mutational burden
TMB in binned analyses defined
- Low TMB as ≤5,
- Intermediate TMB >5 and <20,
- High TMB as ≥20 and <50, and
- Very high TMB as ≥50 mutations/Mb
Tumor mutation burden looks for the number of mutations that are in a tumor that can change proteins in a patient’s tumor cells. For immunotherapies to be effective, the immune system has to recognize one of these abnormal proteins. That is why it is thought that having more mutations may improve your chance of responding well to immunotherapy. Referenced Article
TMB is an in-house next generation sequencing platform which is able to accurately assess the number of DNA mutations in a tumour cell’s genome. The total number of mutations found in the DNA of cancer cells is called the Tumour Mutational Burden.
Immunotherapy works by activating the immune cells to target the neoantigens to kill the cancer cell.
The higher the tumour mutation burden, the greater the numbers of neoantigens expressed on the surface of tumours cells and therefore the more effective the attack by the immune system on these cancer cells will be.The tumour mutation burden is therefore an indicator of how patients are likely to respond to immunotherapy. The higher the tumour mutation burden the more likely the tumour will respond to immunotherapy – Referenced Article
What are neoantigens? Neoantigens are newly formed antigens that have not been previously recognized by the immune system. Neoantigens can arise from ….Recently, a high tumor mutational burden (TMB) has been identified as a genetic signature that is associated with a favorable outcome for immune checkpoint inhibitor therapy. The TMB is defined as the total number of nonsynonymous mutations per coding area of a tumor genome. Initially, it was determined using whole exome sequencing, but due to the high costs and long turnaround time of this method, targeted panel sequencing is currently being explored to measure TMB. In the near future, TMB evaluation may play an important role in immuno-oncology, but its implementation in a routine setting involves robust analytical and clinical validation. Standardization is also needed in order to make informed decisions about patients. This review presents the methodologies employed for determining TMB and discusses the factors that may have an impact on its measurement. Referenced article
Also
High Tumor Mutational Burden Correlates with Longer Survival in Immunotherapy-Naïve Patients with Diverse Cancers
Higher tumor mutational burden (TMB) has been correlated with response to checkpoint blockade immunotherapy. However, it is unclear whether TMB independently serves as a prognostic biomarker for outcomes in immunotherapy-naïve patients. Here, we evaluated the relationship between TMB and overall survival in 1,415 immunotherapy-naïve patients with diverse advanced malignancies. TMB was studied both as a tiered variable (low ≤5 mutations/Mb, intermediate >5 and <20, high ≥20 and <50, and very high ≥50) and as a continuous variable. Interestingly, we observed a parabolic correlation between TMB and overall survival, in which intermediate-range TMB correlated with decreased survival, whereas low and very high TMB correlated with improved outcomes (median survival: 238, 174, 195, and 350 weeks for low, intermediate, high, and very high TMB, respectively; multivariate P < 0.01). This corresponded to an HR of 1.29 (95% confidence continue reading
Tumor Mutation Burden and Cancer Treatment
JAMA Oncology Patient Page
December 17, 2020
Referenced article
https://jamanetwork.com/journals/jamaoncology/fullarticle/2773840
What Is Tumor Mutation Burden?
The goal of cancer treatment is to kill cancer cells while not hurting the body’s healthy cells. One way this is done is by using a drug to target a specific genetic change (also referred to as a mutation) in the cancer cells that is not seen in healthy cells. Historically, many of these mutations have been associated with an aggressive biology and sometimes resistance to cancer treatments, such as chemotherapy. But with immunotherapy, which is treatment given to stimulate or remove inhibition of the immune system to help combat a cancer, a higher number of mutations in a tumor can also be associated with a greater probability of response to treatment. This is because the immune system has a better opportunity to attack the cancer effectively if it can recognize it, and the body’s immune system may better identify cancer cells that have a higher number of mutations.
Here, the number of mutations is like lottery tickets. Although buying a large number of lottery tickets does not mean you will always have a winning ticket, it increases the chance of winning compared with only buying 1 or 2 tickets. Similarly, if a tumor has many different mutations, the odds are greater that the immune system will be able to recognize at least 1 of these mutations and kill the cancer (win the lottery). The number of mutations in a tumor cell is commonly referred to as the tumor mutation burden (TMB) of the cancer.
Measuring TMB
- The TMB can be measured by a laboratory test that uses next-generation sequencing of tumor tissue, which looks broadly for a wide range of mutations.
- Although not as established as measuring TMB from a biopsy sample of tumor tissue, studies are now evaluating measuring TMB from circulating tumor DNA in the plasma, making it potentially possible to test TMB from blood in the future.
- The TMB is reported as the number of mutations seen in a section of DNA and reported as mutations per megabase (mut/Mb).
- Cancers with a TMB of 10 mut/Mb or greater (called TMB-high) may be more likely to respond to drugs called immune checkpoint inhibitors that help activate the immune system to better recognize cancer cells.
Current Role of TMB in Cancer Therapy
The TMB can be helpful in predicting response to immune checkpoint inhibitor treatment across many cancer types. However, it may be a better predictor for some cancers and not as helpful for others. Clinical trials are being conducted now to understand which cancers with high TMB respond best to drugs that help turn on the immune system. The immune checkpoint inhibitor pembrolizumab is approved for treating both adults and children with advanced cancers that have a high TMB (defined as ≥10 mut/Mb) after other drugs have been tried.

October 29, 2020
Prevalence of High Tumor Mutational Burden and Association With Survival in Patients With Less Common Solid Tumors
Key Points
Question What is the prevalence of high tumor mutational burden (TMB-H), defined as 10 or more mutations per megabase, and what is its association with overall survival among patients with 10 rare solid tumor types not treated with immunotherapy?
Findings In this cohort study among 2589 patients, nearly 13% had TMB-H tumors. Overall survival among patients with TMB-H tumors did not differ from that observed among patients with non–TMB-H tumors when receiving nonimmunotherapy treatments.
Meaning These findings suggest that TMB-H was not associated with overall survival in patients with these cancer types in the absence of immunotherapy.
Abstract
Importance Tumor mutational burden (TMB) is a potential biomarker associated with response to immune checkpoint inhibitor therapies. The prognostic value associated with TMB in the absence of immunotherapy is uncertain.
Objective To assess the prevalence of high TMB (TMB-H) and its association with overall survival (OS) among patients not treated with immunotherapy with the same 10 tumor types from the KEYNOTE-158 study.
An association between TMB-H and improved efficacy of immunotherapies has been reported in several tumor types, suggesting TMB-H may be a potential biomarker associated with response to these treatments.7,13,30 An analysis of the KEYNOTE-158 study using the F1CDx assay evaluated associations between TMB and outcomes with pembrolizumab monotherapy. Findings from the KEYNOTE-158 study18 indicated an improved ORR among patients with TMB-H (≥10 mut/Mb) after pembrolizumab monotherapy in the same tumor types as those included in the current study, reporting an ORR of 29% among patients with TMB-H (28% when MSI-H patients were excluded) compared with 6% for patients without TMB-H. Median OS for TMB-H was 11.7 (95% CI, 9.1-19.1) months compared with 12.8 (95% CI, 11.1-14.1) months for patients without TMB-H,19 although the many potential confounding factors associated with assessments in such pooled estimates of OS must be noted. In the context of a single-group study, such as KEYNOTE-158,18 it can be difficult to evaluate whether differences in outcomes (or lack thereof) are representative of a predictive or prognostic association. Our results suggest that assessment of any difference in outcomes by TMB status in KEYNOTE-158 was not confounded by a prognostic association of TMB-H.
The association between TMB-H and clinical outcomes may further be strengthened by co-occurrence of another marker of genomic instability, such as MSI-H.21,31 Chalmers et al21 reported that 97% of specimens with MSI-H also had TMB-H and that such co-occurrences are observed more frequently in certain cancer types, especially in gastrointestinal cancers, but rarely in melanoma and lung carcinoma. As such, comparative analysis of biomarkers associated with treatment response and their association with rare solid tumor types may help provide accurate and improved usage of immunotherapies.
full article https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2772345
TMB-H had the same cutoff used for the KEYNOTE-158 analysis18 (ie, ≥10 mut/Mb), but for an additional exploratory analysis, the cutoff was 13 or more mut/Mb, a threshold that has been evaluated in other clinical trials.11
Testing and Profiling
IHC Immunohistochemical testing and Molecular Profiling the whole genome
Test ID: IHC
Mismatch Repair (MMR) Protein Immunohistochemistry Only, Tumor
IHC alone can determine retention or loss of MLH1, MSH2, MSH6, and PMS2 protein expression. If all 4 proteins are present,
Link
www.mayocliniclabs.com/test-catalog/Clinical+and+Interpretive/35466
Article by
Cancer.org
IHC stains can help recognize specific substances in cancer cells that influence a patient’s prognosis and/or whether they are likely to benefit from certain drugs.
RNA & mRNA
Types of RNA: mRNA, rRNA, and tRNA
RNA or ribonucleic acid is a polymer of nucleotides that is made up of a ribose sugar, a phosphate, and bases such as adenine, guanine, cytosine, and uracil. It plays a crucial role in gene expression by acting as the intermediate between the genetic information encoded by DNA and proteins.
Messenger RNA (mRNA) is a single-stranded RNA molecule that is complementary to one of the DNA strands of a gene. The mRNA is an RNA version of the gene that leaves the cell nucleus and moves to the cytoplasm where proteins are made. . . read more
Messenger RNA (mRNA) is a single-stranded RNA molecule that is complementary to one of the DNA strands of a gene. The mRNA is an RNA version of the gene that leaves the cell nucleus and moves to the cytoplasm where proteins are made. . . read more
ncbi.nlm.nih.gov/pmc/articles
“RNA-based vaccines have become potentially promising as alternative approaches to conventional vaccine development… In summary, self-amplifying RNA virus vectors have been subjected to a large number of preclinical studies for both infectious diseases (Table 1) and different types of cancers …”
“…demonstrated tumor regression and prolonged survival. As most of the clinical trials conducted so far have comprised phase I studies, the focus has mainly been on safety and tolerability. Despite that, prolonged survival was established in pancreatic cancer patients treated with VEE-CEA [150], stable disease in ovarian cancer patients immunized with MV-CEA [149] and complete remission in one patient with refractory multiple myeloma after treatment with MV-NIS [148]. However, in many of the studies the immune responses were relatively modest, suggesting that optimization of doses, prime-boosting, vector choice and delivery method/route are necessary.”
“…In attempts to enhance immune responses for development of better vaccines, attention has also been paid to vector engineering and delivery improvements. Oncolytic viruses have been applied for specific infection of tumor cells, leading to their killing without affecting normal tissues [160]. Another approach involves liposome- and polymer-encapsulation strategies with the goals of tumor targeting and protection against degradation and recognition by the host immune system….”
“…For instance, liposome encapsulated SFV particles demonstrated tumor targeting and allowed repeated administration in cancer patients …”
“…n conclusion, self-amplifying RNA virus vectors provide the flexibility of utilizing RNA replicons, recombinant VLPs or DNA replicon plasmids for immunization studies leading to robust antibody responses and protection against challenges with lethal doses of pathogens or tumor cells. Although so far, clinical responses have been relatively modest, vector development, dosage optimization and delivery improvement will support the production of efficient vaccines in the near future. These needs are even more crucial today with the current COVID-19 pandemic….” read more
Virus
Comments
BASIC INFORMATION ON THE STRUCTURE, FUNCTION AND REPLICATION OF A VIRUS
Contact us: contact@5minuteschool.com
Lightweight opinion information direction = correct – superficial seeking public acceptance – not science
…”mRNA vaccines have many benefits. They are quick to design, so once the manufacturing platform is set up, mRNA vaccines can be designed to target viruses, or variants, very quickly. The vaccine manufacturing is also fully synthetic, and doesn’t rely on living cells like chicken eggs, or cultured cell lines….” read more…
Questions over downstream health impacts.
Article link
‘Ordinarily, two months is way shorter than it would normally take to assess phase 3 trial results,’ he said.
‘But no one’s going to be happy if we say, “Yeah, we’ll get a vaccine to you in five years”. So it’s a risk–benefit analysis…..”‘Now, of course, none of this will tell you if there’s going to be a problem that might crop up a year later, and there’s no way around that other than wait for a year or two years or five years or however long any longer term potential problems might take…”
According to Dr Marks, safety is what ‘keeps [him] up at night’.
‘The way we’re going to get over COVID-19 is if we get a vaccine that has 70% or 80% efficacy and we can deploy that to 70 or 80% of the population,’ he said.
‘[That way] we actually have a chance of having herd immunity, and we can be back in restaurants and in banks … and doing what we normally do.
‘[But] it’s only going to happen if people have confidence enough to go get vaccinated, and we do have a crisis in vaccine confidence.’
University of Sydney vaccine expert Professor Robert Booy told newsGP ‘past experience’ suggests a vaccine candidate is unlikely to produce a serious side effect beyond about two months….
(Steve) this is the very same risk assessment offered up via Ipi/Nivo and keytruda – recent findings in trial cohorts of >200 patients showed 48% of patients did not develop downstream thyroid dysfunctions/lesions at 18 months – but observed that the more successful performing patients did develop downstream impacts – most probably due to overgrowth from amplifications to induce a larger immune response – also separately – replicon mRNA are 3 times larger than native mRNA.
Professor Booy said he is not ‘massively concerned’ about the safety of the two mRNA candidates, but does still hold some reservations.
‘I’m still a bit nervous about mRNA because it’s so new – and it’s so new that we can’t even speculate what it’s going to cause,’ he said.
‘That’s why I suggest the best quality phase 4 post-marketing surveillance, with follow-up at three months after vaccination and six months. Then you’ll have the kind of quality reassurance to go on with the program.’
‘There are chronic effects as well, in a minority of people, and again, it can affect the heart, the lungs, the brain and the kidneys in a chronic way.
‘I don’t want either of those downsides.’
Social Media Impact
Research on what part Social Media plays on research
2011
Social network sites have been growing in popularity across broad segments of Internet users, and are a convenient means to exchange information and support. Research on their use for health-related purposes is limited.
Online communities present a convenient means to exchange information and support with people in similar circumstances and are increasingly being used for health purposes
While young adults are still more likely to use social network sites [5], the fastest growing demographic of Facebook users is women 55 years and older [6], which corresponds to the average age of onset of breast cancer [7]. Although recent studies indicate that Facebook groups are used for health purposes [8], little is known about how this resource is used by people affected by breast cancer.
Social network sites are differentiated from other online communities based on their ability to enable users to display their social networks. Their backbone consists of visible user profiles that display an articulated list of friends who are also users of the system [12]. While other online community platforms enabled users to create a list of friends, these networks were not displayed or accessible to other users. This unique feature of social network sites is hypothesized to result in connections between individuals that would not otherwise have been made [12].
Qualitative studies have revealed that these types of online communities provide breast cancer survivors with a safe, relatively anonymous space to communicate about sensitive and potentially stigmatizing topics [13], reduce feelings of isolation and uncertainty regarding prognosis and ambiguous painful symptoms [14], and enable them to become more informed and better prepared for their interactions with the health system [15]. Randomized controlled trials have shown that professionally moderated mailing lists and message boards for breast cancer survivors can reduce depression, stress, and cancer related trauma, and can enhance social support
Relatively little is known about the use of social network sites for health purposes.
ZAGH Research
General Research – Market
Genomic Cancer Panel and Profiling Markets by Cancer and Germline/Somatic Type with Screening Potential Market Size, Customized Forecasting/Analysis, and Executive and Consultant Guides 2021-2025
Cancer Gene Panels and Genomic Profiling are quickly changing the diagnosis and treatment of cancers. The market is moving out of a specialized niche and going mainstream as Oncologists begin routinely using information on the hundreds of genes related to cancer. The market is exploding as physicians use all the information they can get in the battle against cancer. And there is a lot of information to be had. But the COVID-19 Pandemic has impacted the market. Find out how in this thorough report.
Comprehensive panels, genomic profiling, high-risk breast cancer panels. Learn all about how players are jockeying for position in a market that is being created from scratch. And some players are already taking the lead. It is a dynamic market situation with enormous opportunity where the right diagnostic with the right support can command premium pricing. And the science is developing at the same time creating new opportunities with regularity. And the cost of sequencing continues to fall.
This report provides data that analysts and planners can use. Hundreds of pages of information including a complete list of Current 2020 United States Medicare Fee Payment Schedules to help understand test pricing in detail. Forecast demand for new testing regimes or technologies. Make research investment decisions. Existing laboratories and hospitals can use the information directly to forecast and plan for clinical facilities growth.
The report includes detailed breakouts for 18 Countries and 4 Regions. A detailed breakout for any country in the world is available to purchasers of the report.
“We now know of hundreds of genes, that when mutated, drive cancer. This research shows that across cancer types a relatively consistent small number of such mutated genes is required to convert a single normal cell into a cancer cell, but that the specific genes chosen differ according to cancer type. The study also shows that we have not yet identified many of these driver genes and they will be the target for further searching in the future. This increasingly precise understanding of the underlying changes that result in cancer provides the foundation for the discovery and use of targeted therapies that treat the disease.”
Professor Sir Mike StrattonAn author of the study and director of the Wellcome Trust Sanger Institute
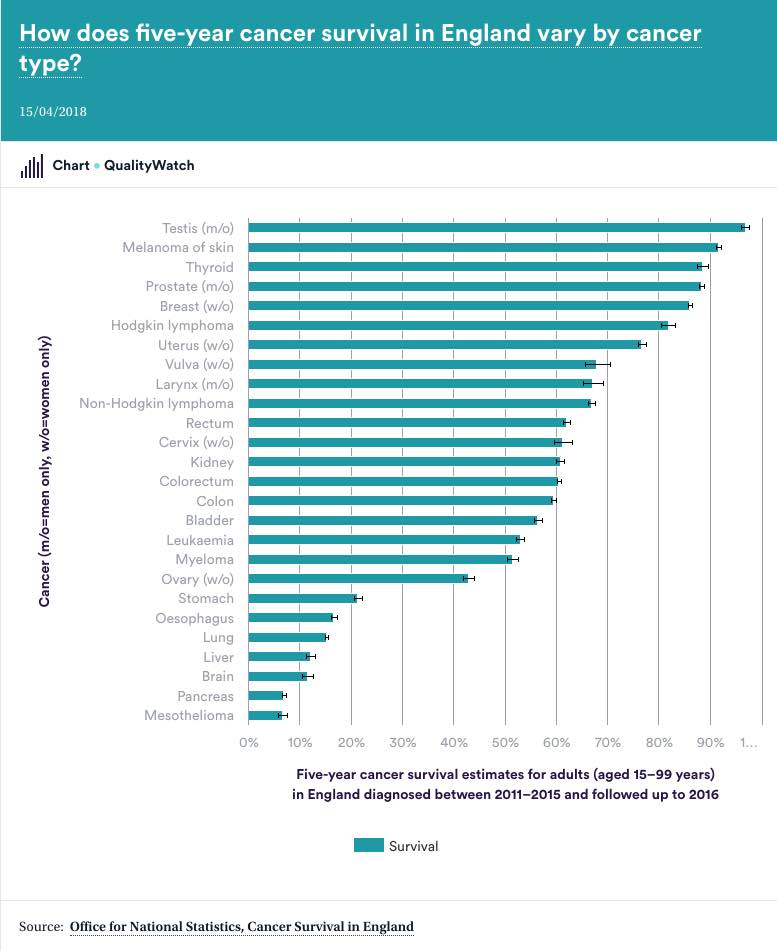
An Audit on Cancer
On Nightlife with Suzanne Hill